
By Angeli Chitale, BSc, ND, Canada
What is Stress? Stress is a threat to the internal balance (homeostasis) of the body. Stress related conditions including anxiety, depression, high blood pressure, indigestion, reflux, and peptic ulcer disease can be interpreted as consequences of body’s inability to maintain internal balance in response to internal or external demands. Stress impairs digestion, decreases immune function and alters mood (anxiety and depression). We will focus on digestion since health and illness begin in the gut!
Gut-Brain Connection and Stress: The impact of stress on health is well studied and documented. A large nerve network in our stomach and intestines is constantly making chemicals in response to signals from the (internal and external) environment. Brain chemicals such as serotonin, are made in the gut and travel to the brain. When our brains see serotonin = feel good, we feel “ahh, all is well, I can relax”. The gut is called the “second brain” for this reason and medical research is pointing to many ways stress interferes with digestive function.
Symptoms of Impaired Digestive Function:
- Bloating, gas
- IBS
- Constipation and diarrhea,
- Pain / abdominal discomfort,
- Fatigue,
- Blood sugar imbalances (seen as food cravings or emotional if delayed or missed meal),
- Food sensitivities and “leaky gut” and even weight gain
These symptoms interfere with the quality of daily life as the leading reason for visits to the doctor’s office are for abdominal pain / digestive issues.
How Can All of the Above Symptoms be Provoked by Stress? One study of caregivers of brain cancer patients found that even when there was no evidence of elevated stress hormones (adrenaline and cortisol made by the adrenal glands), there was another way to measure the stress response. This time in white blood (immune) cells. The study found white blood cells (monocytes) became resistant to another adrenal hormone - glucocorticoids, when the body was under stress. Glucocorticoids are your body’s natural anti-inflammatories. Glucocorticoid resistance allows activation of chemicals which promote inflammation such as NfKB.
Another study found that key elements of intestinal function - digestion, absorption, and barrier function, are impaired during inflammation. Chronic inflammation can lead to damage of the lining of the digestive tract altering digestion, absorption, and barrier function.
Bottom line: Under stress, natural anti-inflammatories are suppressed and inflammation promoting chemicals are increased. Inflammation impairs digestive function by interfering with digestion (breaking down of food into molecules), absorption, and barrier function.
What We Can do to Alter the Stress Response
Slow Down Before Eating: Give thanks before eating your meal. Take a few minutes to appreciate the connection to life and sustenance with the food you are about to eat. Scientifically, this action brings you out of sympathetic dominance (the stress response) and prepares your body for parasympathetic mode (rest and digest).
Herbal Nerve Tonics:
Gentle nervine (nerve tonic) herbs specifically address stress related digestive impairment and can be safely taken daily as a medicinal infusion (strong tea) throughout the day.
Catnip (Nepeta cataria): Mild antispasmodic for soothing pain from digestive cramping
Chamomile (Matricaria recutita): Soothes digestive colic and irritability
Peppermint (Mentha piperita): The aromatic oils help soothe symptoms of IBS and gas
Herbal Anti-Inflammatories:
Turmeric and Ginger roots have been used in Ayurvedic Medicine for thousands of years.
Make a decoction (boiling the roots to make an extraction) and drink as a tea to break the cycle of inflammation.
Nutrients:
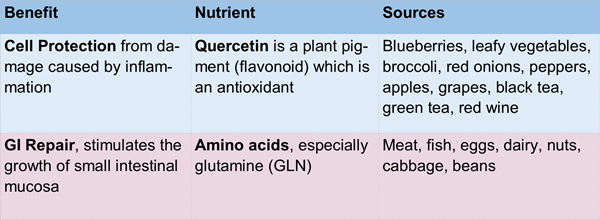
Studies have shown specific nutrients to protect and / or repair the intestinal mucosa (lining) from the damage caused by inflammation.
References: 1. A Functional Genomic Fingerprint of Chronic Stress in Humans: Blunted Glucocorticoid and Increased NF-κB Signaling. 2. Biological Psychiatry. Volume 64, Issue 4, 15 August 2008, Pages 266-272 3. Inflammation and intestinal function: where does it start and what does it mean? JPEN J Parenter Enteral Nutr. 2008 Nov-Dec;32(6):648-50. doi: 10.1177/0148607108325177.







